Artificial insemination with the partner’s semen
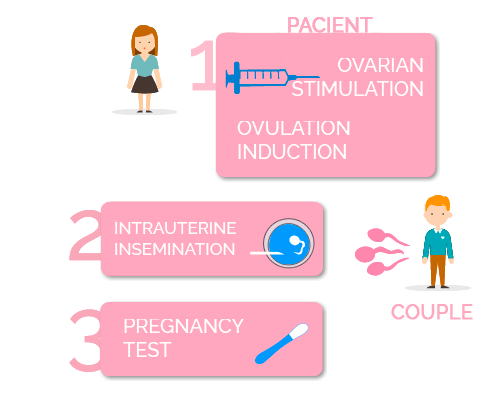
In vitro fertilization (IVF) with the partner’s sperm, also known as intrauterine insemination with the partner’s sperm, is a technique where sperm from the partner is deposited in the woman’s uterus during her ovulation period, with the objective of facilitating pregnancy. It is the simplest assisted reproduction technique.
What does Artificial Insemination with the partner’s semen consist of?
For whom is this technique indicated?
Artificial Insemination with the partner’s semen is indicated for
- Couples where the woman has ovulatory dysfunctions such as polycystic ovary síndrome (PCOS), anovulation (not releasing an egg each month) or problems in the follicular phase, but an acceptable ovarian reserve, permeable fallopian tubes, and normal quality – or with mild-moderate alterations – of the partner’s semen
- Couples where the woman has mild or moderate endometriosis.
- Couples where the woman suffers from cervical mucus defect.
- Couples where the woman has anatomical alterations, such as stenosis (narrowing of the cervix) or vaginismus.
- Couples where the man cannot deposit the semen in the vagina: sexual impotence, retrograde ejaculation, premature ejaculation.
- Couples with immunological sterility problems, where antibodies are produced in the female reproductive system that destroy spermatozoa.
The requirements for a couple to undergo artificial insemination and have the best chance of success are:
- To check the permeability of the fallopian tubes to ensure the passing of sperm for fertilization to take place, and consecutively for the zygote to reach the uterus.
- To have an ultrasound scan done to rule out possible uterine malformations that could affect the implantation and development of the pregnancy. In addition, to ensure that the ovary is capable of responding to stimulation enabling the retrieval of a minimum of oocytes suitable for the performance of the technique.
- To establish with semen analysis that there is a minimum quality of semen. The couple’s semen sample must meet minimum concentration and/or mobility requirements.
- To ensure that there is no risk of contagion to the partner and/or future baby, ruling out the risk of possible hepatitis C or B, HIV, rubella (german measles), syphilis and toxoplasmosis.
- The age of the woman directly influences the chances of success or failure. The chances of pregnancy using this technique begin to decrease when a woman approximately reaches 36.
40% Cumulative rate
According to the Spanish Fertility Society (SEF) registry, Spain is currently the third country in Europe with the most artificial insemination treatments. Some 23,000 inseminations are performed each year.
Usually, after the insemination, the patient waits for about an hour in the room at the assisted reproduction center. Then, once at home, the woman can lead a normal life.
Once gestation is achieved, the development of the pregnancy is totally normal; the risk of miscarriage, premature delivery, or for the baby to be born with a congenital anomaly is the same as in a pregnancy obtained through vaginal intercourse.

