Ovodonation with donor sperm
Egg donation with sperm from a donor is a technique whereby a healthy young woman decides to donate her eggs, anonymously and altruistically, to assisted reproduction centers so that they can be used by other women or couples who have female fertility problems.
These donated eggs are fertilized in the laboratory by the sperm of a carefully selected anonymous donor. The correctly fertilized ones are monitored for several days until the best quality embryos are transferred to the maternal uterus. It is the most effective assisted reproduction technique, thanks to its high pregnancy rates.
What does egg donation with donor sperm consist of?
In the egg donation process, a healthy young woman decides to altruistically donate her oocytes to assisted reproduction centers so that other women or couples with female fertility problems can achieve pregnancy.
The egg donor must meet certain requirements to be part of the egg donation program. They must:
- be between 18 and 35 years old,
- be in perfect health, both physical and mental
- have a family medical history that guarantees that they will not transmit genetic or hereditary diseases or congenital malformations,
- go through an examination that guarantees they will not transmit any disease of sexual or infectious nature,
- submit themselves to a fertility study,
- can only be a donor for a total of 6 living babies, counting donations and their own children.
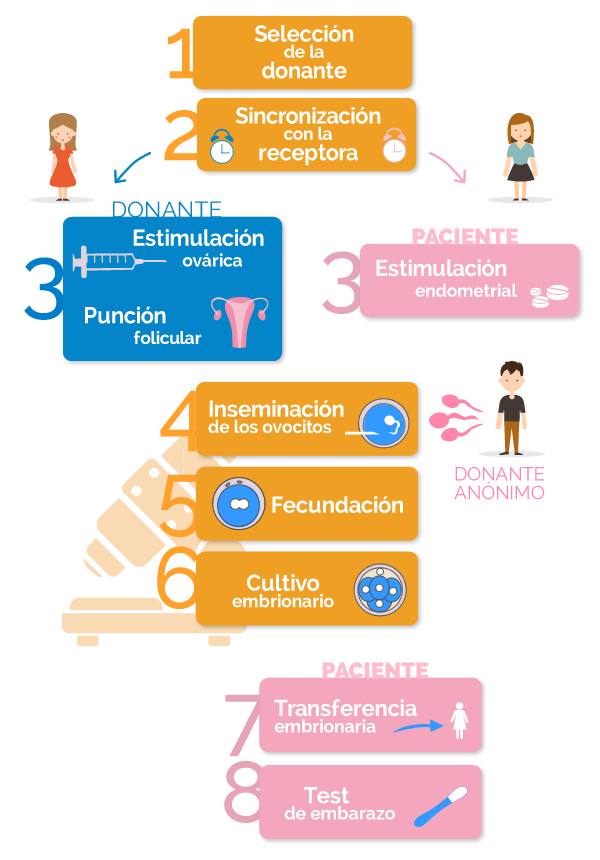
For the in vitro fertilization treatment with egg donation to be successful, the menstrual cycles of the donor and the recipient must be synchronized.
The donor will start taking an anovulant that will be withdrawn before starting the ovarian stimulation.
The egg donor woman will undergo ovarian stimulation, with the use of gonadotropin hormones similar to those produced by the woman herself. The donor will thus manage to develop several follicles to obtain several oocytes during the cycle. This ovarian stimulation will be periodically monitored with ultrasound scans and blood tests.
Once several follicles have reached the appropriate size, approximately 18mm in diameter, the hCG hormone will be administered to trigger the final maturation of the oocytes.
Follicular puncture is performed by a fertility specialist, who will extract the mature oocytes through the vagina. The donor will remain sedated during the process, since the procedure is minimally invasive, lasts less than 15 minutes and allows the patient to immediately return to normal activity.
Meanwhile, the recipient of the eggs must follow an endometrial preparation treatment in order to receive the embryos.
The recipient woman will be administered an injection of a GnRH analog on day 22 of the menstrual cycle to desensitize the pituitary gland. When the menstruation starts, the recipient will have to start an estrogen treatment, in increasing doses, to achieve the appropriate endometrial thickness, which will be assessed through vaginal ultrasound scans. Once the endometrium has grown, the recipient is ready for the transfer of embryos.
On the day of the donor follicular puncture, the oocytes will be retrieved and inseminated by sperm from a semen sample obtained from an anonymous donor.
Depending on the characteristics of the semen sample used and the patient’s history, insemination will be performed by conventional IVF and/or ICSI.
In conventional IVF, retrieved donor oocytes and the most capable sperm from the anonymous donor are placed in contact in a laboratory dish, and one of them is expected to fertilise the donor oocyte.
With ICSI (intracytoplasmic sperm injection), the embryologist inserts a sperm selected from the anonymous donor’s semen sample into each oocyte with the help of a micromanipulator and a microneedle, directly in the laboratory.
The correctly fertilized embryos will be kept in the laboratory under observation for several days. During this time, the division of the embryos into an increasing number of cells will be monitored.
The resulting embryos that have the appropriate morphological characteristics will be the ones transferred to the uterus of the recipient woman, and if there are spare, they will be frozen.
The appropriate number of embryos to be transferred will be decided on the day, the maximum being three per cycle.
The gynecologist will use a small catheter to guide the embryos through the cervix and into the uterus. The embryo transfer procedure lasts a few minutes and the patient recovery time is minimal.
The pregnancy test will be carried out by means of a blood test 13 days after the follicular puncture of the donor. If the patient suffers from bleeding before the test, it is important that she never stops taking the medication and that she seeks advice from the medical team.
Throughout the artificial insemination treatment, her personal assistant will be available at all times to answer any questions she may have and support her in this very special moment.
For whom is this technique indicated?
Egg donation with donor semen is indicated for:
- Couples where the man has severe male factor infertility, with poor sperm quality or azoospermia.
- Couples where the man is the carrier of a genetic disease that cannot be diagnosed by PGD.
- Couples where the woman suffers from ovarian failure due to menopause, premature ovarian failure or ovarian surgery.
- Couples where the woman is elderly.
- Couples where the woman cannot use her own oocytes, because of their poor quality.
- Couples where the woman has experienced repeated implantation failures in In Vitro Fertilisation treatments.
- Couples where the woman has undergone surgery, chemotherapy and radiotherapy treatments.
- Couples where the woman has chromosomal alterations and serious hereditary diseases that cannot be detected by PGD techniques.
- Couples who have suffered recurrent miscarriages.
- Couples who have failed other previous assisted reproduction techniques.
- Women without a male partner who want to get pregnant and be single mothers.
- Couples of homosexual women.
At VITA we have a team of specialists in charge of carrying out the selection process of oocyte donors and their subsequent coordination with the recipient patients.
Where do egg donors come from?
According to the Spanish legislation on donations, egg donors must meet some requirements. They must be between the ages of 18 and 35, in good mental and physical health, and free of any genetic or sexually transmitted disease.
The donors are young women who freely decide to carry out an altruistic and anonymous act of solidarity to help other women fulfill their dream of becoming mothers. All donors go through a “Donor Screening“, a rigorous medical and psychological examination to guarantee the highest quality and safety in the treatments.
Donors undergo a complete medical check-up where diseases, family history and personal habits are evaluated. A psychological test, a gynecological examination, an ultrasound scan and blood tests are carried out, as well as a genetic study of autosomal recessive diseases carriers.
If all the tests are satisfactory, the donor is included in our donor database until there is a possible recipient compatible with her phenotype (physical characteristics).
Where do sperm donors come from?
According to the Spanish legislation on donations, semen donors must meet some requirements. They must be between 18 and 35 years old, in good mental and physical health, have good semen quality and not suffer from any genetic or sexually transmitted disease.
VITA uses the CEIFER sperm donor bank, whose donors go through a strict and exhaustive examination in order to guarantee the quality of the treatments. The donor will undergo various tests and studies, such as a first medical evaluation, a psychological test, a study of the sperm quality, a genetic study and a study of infectious diseases, sexually transmitted diseases, etc.
All sperm donors go through the “Donor Screening“, a Study of Autosomal Recessive Genetic Diseases Carriers. Through this test it is possible to detect the most common autosomal recessive genetic diseases. In addition, when the time comes to assign the donor, a “Genetic Matching” protocol is followed, so that the donor and the patient do not share mutations in the same genes.





