Artificial insemination with donor semen (IUI/DI or Heterologous Insemination)
Artificial insemination with donor semen, also known as intrauterine insemination with donor semen (IUI/DI or heterologous insemination) is a technique in which the sperm of an anonymous donor from a sperm bank are deposited in an unnatural way in the uterus of the woman during her ovulation phase, with the aim of facilitating pregnancy.
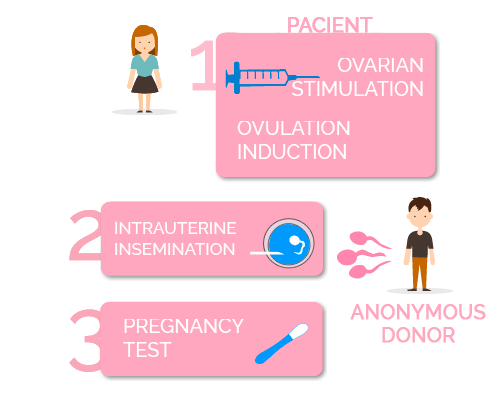
What does Artificial Insemination with donor semen consist of?
For whom is this technique indicated?
Artificial Insemination with donor semen is indicated for
- Couples where the man presents severe alterations in seminal parameters or presents azoospermia, the absence of sperm in the ejaculate.
- Couples where the man is the carrier of a genetic disease that cannot be diagnosed by PGD (Preimplantation Genetic Diagnosis).
- Couples who have failed other previous treatments, such as IVF-ICSI with the partner’s semen, due to a very severe male factor infertility.
- Couples at risk of transmitting sexually transmitted diseases, such as Hepatitis B, Hepatitis C, Syphilis or AIDS.
The requirements for a couple to undergo artificial insemination and have the best chance of success are:
- To check the permeability of the fallopian tubes to ensure the passing of sperm for fertilization to take place, and consecutively for the zygote to reach the uterus.
- To have an ultrasound scan done to rule out possible uterine malformations that could affect the implantation and development of the pregnancy. In addition, to ensure that the ovary is capable of responding to stimulation enabling the retrieval of a minimum of oocytes suitable for the performance of the technique.
- To Select a semen sample from an anonymous donor bank with adequate sperm count and motility parameters, selected with a “Donor Screening” protocol that detects autosomal recessive genetic diseases.
- To ensure there is no risk of contagion to the partner and/or future baby, ruling out the risk of possible hepatitis C or B, HIV, rubella (German measles), syphilis and toxoplasmosis.
- The age of the woman directly influences the chances of success or failure. The chances of pregnancy using this technique begin to decrease when a woman approximately reaches 36.
Once gestation is achieved, the development of the pregnancy is totally normal; the risk of miscarriage, premature delivery, or for the baby to be born with a congenital anomaly is the same as in a pregnancy obtained through vaginal intercourse.
Where do sperm donors come from?
According to the Spanish legislation on donations, sperm donors must meet certain requirements. They must be between 18 and 35 years old, in good mental and physical health, have good semen quality and not suffer from any genetic or sexually transmitted disease.
VITA uses the CEIFER sperm donor bank, whose donors go through a strict and exhaustive examination in order to guarantee the quality of the treatments. The donor will undergo various tests and studies, such as a first medical evaluation, a psychological test, a study of the sperm quality, a genetic study and a study of infectious diseases, sexually transmitted diseases, etc.
All sperm donors go through the “Donor Screening“, a Study of Autosomal Recessive Genetic Diseases Carriers. Through this test it is possible to detect the most common autosomal recessive genetic diseases. In addition, when the time comes to assign the donor, a “Genetic Matching” protocol is followed, so that the donor and the patient do not share mutations in the same genes.

